The Pain Catastrophizing Scale (PCS) is a self-report questionnaire assessing cognitive and emotional responses to pain, focusing on rumination, magnification, and helplessness․ Widely used in clinical settings, it helps quantify pain experiences and guides therapeutic interventions․
Definition and Overview
The Pain Catastrophizing Scale (PCS) is a self-report measure assessing catastrophic thinking about pain․ It evaluates how individuals experience and interpret pain through three subscales: rumination, magnification, and helplessness․ The scale consists of 13 statements, with respondents rating their thoughts and feelings on a 5-point scale․ Total scores range from 0 to 52, higher scores indicating greater catastrophizing․ Widely used in clinical and nonclinical populations, the PCS provides insight into pain-related cognitive and emotional processes, aiding in understanding and managing chronic pain․ Its application helps identify negative pain schemas and inform therapeutic interventions tailored to individual needs․
Importance of Assessing Pain Catastrophizing
Assessing pain catastrophizing is crucial for understanding how individuals process and cope with pain․ The PCS identifies negative thought patterns, such as rumination and magnification, which can exacerbate suffering․ Early identification helps prevent chronic pain and mental health issues like anxiety and depression․ By evaluating these cognitive and emotional responses, healthcare providers can tailor interventions, improving treatment outcomes and enhancing quality of life for individuals with pain conditions․
Development and History of the PCS
The PCS was developed by Michael J․L․ Sullivan, PhD, to measure catastrophic thinking in pain experiences․ First introduced in 1995, it has since become a widely used tool in pain research and clinical practice, aiding in understanding the cognitive and emotional aspects of pain perception․
Creation and Evolution of the Scale
The Pain Catastrophizing Scale (PCS) was created by Michael J․L․ Sullivan, PhD, to assess catastrophic thinking in pain․ Initially developed in 1995, it has undergone revisions, enhancing its validity and reliability․ The scale’s evolution reflects advancements in understanding pain cognition, ensuring it remains a robust tool for clinical and research applications, helping to identify maladaptive thought patterns that exacerbate pain experiences․
Original Author and Purpose
The Pain Catastrophizing Scale (PCS) was developed by Michael J․L․ Sullivan, PhD, a prominent researcher in pain psychology․ Its primary purpose is to measure catastrophic thinking patterns in individuals experiencing pain․ Sullivan aimed to create a tool that could quantify pain-related cognitions and emotions, aiding clinicians and researchers in understanding how these factors influence pain experiences and treatment outcomes․ The PCS remains a cornerstone in pain assessment, helping identify maladaptive thought patterns that hinder recovery․
Structure of the Pain Catastrophizing Scale
The Pain Catastrophizing Scale (PCS) consists of 13 items, divided into three subscales: Rumination, Magnification, and Helplessness․ It assesses cognitive and emotional responses to pain experiences․
Subscales: Rumination, Magnification, and Helplessness
The PCS includes three subscales: Rumination, assessing preoccupation with pain, Magnification, evaluating exaggerated threat beliefs, and Helplessness, measuring perceived inability to cope․ These dimensions provide insights into cognitive and emotional pain responses, aiding in tailored interventions and understanding the complexity of pain experiences in clinical populations․ Each subscale contributes uniquely to the overall assessment of catastrophic thinking patterns․
Number of Items and Response Format
The PCS consists of 13 items, divided into three subscales․ Each item is rated on a 5-point Likert scale, ranging from “Not at all” to “All the time․” Respondents indicate how frequently they experience specific thoughts or feelings when in pain․ The scale is self-administered, making it accessible for both clinical and research settings․ This format ensures a standardized method for quantifying catastrophic thinking patterns, facilitating reliable data collection and scoring processes for clinicians and researchers․

Administration and Scoring of the PCS
The PCS is a 13-item self-report questionnaire using a 5-point Likert scale․ Patients rate their thoughts and feelings during pain, with scores ranging from 0 to 52․ Summing responses provides a total score, helping assess catastrophic thinking severity․ The scale is straightforward to administer in both clinical and research settings, offering valuable insights into pain-related cognitive patterns․
How to Complete the Scale
The PCS is a self-report questionnaire consisting of 13 items․ Patients rate their thoughts and feelings during pain on a 5-point Likert scale (0 = “Not at all,” 4 = “All the time”)․ Each item reflects catastrophic thinking, such as ruminating on pain or feeling helpless․ Respondents select the option that best describes their experience․ The scale is typically completed in 5-10 minutes and can be administered in clinical or research settings․ Instructions are provided to ensure clarity and accuracy․
Scoring System and Interpretation
The PCS consists of 13 items, each scored on a 5-point Likert scale (0 = “Not at all” to 4 = “All the time”)․ The total score ranges from 0 to 52, with higher scores indicating greater catastrophizing․ Subscales assess rumination, magnification, and helplessness․ Scores are calculated by summing responses, and interpretations guide clinical decisions․ Elevated scores suggest increased risk of chronic pain and emotional distress, aiding in tailored interventions and progress monitoring․

Clinical Applications of the PCS
The PCS is widely used in clinical settings to assess chronic pain patients’ emotional and cognitive responses, aiding in diagnosis, treatment planning, and monitoring progress effectively․
Assessment of Chronic Pain Patients
The PCS is crucial for evaluating chronic pain patients, providing insights into their cognitive and emotional pain responses․ It helps identify individuals at risk of developing chronic pain and those with heightened distress․ By assessing rumination, magnification, and helplessness, the PCS enables clinicians to tailor interventions, improving pain management strategies and patient outcomes․ This tool is integral in clinical interviews, allowing patients to share their pain experiences and facilitating personalized care plans․
Monitoring Treatment Progress
The PCS is a valuable tool for monitoring treatment progress in chronic pain management․ By tracking changes in cognitive and emotional responses to pain, clinicians can assess the effectiveness of interventions․ Regular administration of the PCS helps identify improvements or deteriorations in patients’ mental state, enabling timely adjustments to treatment plans․ This ongoing assessment supports personalized care and enhances the overall management of chronic pain conditions, ensuring better patient outcomes and tailored therapeutic approaches․

Psychological Impact of Pain Catastrophizing
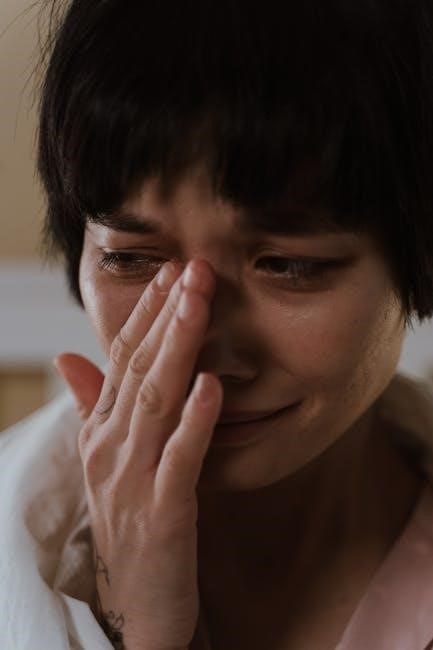
Pain catastrophizing amplifies anxiety, fear, and helplessness, intensifying emotional distress and impairing mental well-being․ It fosters a cycle of negative thoughts, exacerbating the perception of pain and its impact․
Cognitive and Emotional Responses to Pain
The Pain Catastrophizing Scale (PCS) assesses how individuals cognitively and emotionally respond to pain, focusing on rumination, magnification, and helplessness․ These responses involve persistent, negative thoughts about pain, such as believing it will worsen or become unbearable․ Emotional reactions like anxiety and fear intensify the pain experience, creating a cycle of distress․ Such cognitive patterns can amplify suffering, impair mental health, and reduce daily functioning, making them critical targets for intervention in pain management strategies․
Relation to Anxiety, Fear, and Helplessness
Pain catastrophizing is closely linked to heightened anxiety and fear, as individuals often perceive pain as unbearable or worsening․ This mindset fosters feelings of helplessness, intensifying emotional distress․ Such reactions create a cycle where fear of pain exacerbates anxiety, which in turn amplifies pain perception․ The PCS identifies these patterns, aiding in understanding how cognitive and emotional responses contribute to chronic suffering and impaired mental health, emphasizing the need for targeted interventions to break this cycle․
Research Findings and Validation
The PCS has been extensively validated, demonstrating reliability across diverse populations․ Studies confirm its effectiveness in assessing catastrophic thinking and its impact on emotional pain responses․
Studies Supporting the PCS
Research confirms the PCS’s validity in measuring catastrophic thinking․ A study administering the PCS to 425 undergraduates revealed a three-component structure: rumination, magnification, and helplessness․ Findings highlight its reliability across diverse populations, with strong correlations to pain intensity and emotional distress․ Cited by numerous researchers, the PCS is widely recognized as a robust tool for understanding pain-related cognitive processes and their impact on patient outcomes in clinical settings․
Reliability and Validity Across Populations
The PCS demonstrates strong reliability and validity across diverse populations, including chronic pain patients and nonclinical groups․ Studies show consistent internal consistency and construct validity, with correlations to pain intensity and emotional distress․ Cross-cultural adaptations ensure its applicability in various settings, making it a reliable tool for assessing catastrophic thinking in pain experiences globally․ Its robust psychometric properties support its widespread use in both clinical and research contexts effectively․
Cultural and Demographic Considerations
The PCS has been adapted for diverse cultures and demographic groups, ensuring its effectiveness across different backgrounds and languages, making it a versatile tool for global pain assessment․
Adaptations for Different Populations
The PCS has been translated and validated for use in non-English speaking populations, ensuring cultural relevance․ Researchers have adapted the scale to accommodate diverse cultural backgrounds, making it accessible for global use․ These adaptations maintain the original structure while addressing language and conceptual differences, ensuring accurate assessment of pain catastrophizing across varied demographic groups․
Cultural Differences in Pain Perception
Cultural background significantly influences pain perception and catastrophizing․ Studies show that individuals from collectivist cultures may report higher levels of pain-related helplessness․ Language and societal norms shape how pain is expressed and interpreted, affecting PCS scores․ Understanding these differences is crucial for accurate assessment and tailored interventions across diverse populations․
Limitations and Critiques of the PCS
The PCS may exhibit cultural biases and relies on self-reported data, which can be subjective․ It may not fully capture nuanced pain experiences or contextual factors․
Potential Biases and Misinterpretations
The PCS may reflect cultural biases, as pain perception varies across populations․ Its reliance on self-reported data introduces subjectivity, potentially leading to overestimation or underestimation of catastrophizing․ Additionally, the scale’s focus on negative cognitions may overlook adaptive coping strategies, possibly misrepresenting individuals’ overall pain experiences․ These factors highlight the need for cautious interpretation and cultural adaptation when administering the PCS across diverse groups․
Comparison with Other Pain Assessment Tools
The PCS differs from tools like the Visual Analog Scale (VAS) and McGill Pain Questionnaire (MPQ) by focusing on cognitive-emotional responses rather than pain intensity alone․ While other scales measure pain severity or location, the PCS uniquely captures catastrophic thinking patterns․ However, it does not assess pain intensity directly, making it complementary rather than a replacement for other measures․ This distinction highlights its specialized role in understanding psychological dimensions of pain experiences․
Practical Applications Beyond Clinical Settings
The PCS is valuable in occupational health for assessing pain’s impact on work and rehabilitation․ It aids in designing tailored programs to improve functionality and reduce absenteeism effectively․
Use in Occupational Health and Rehabilitation
The PCS is instrumental in occupational health for evaluating how pain impacts employees’ work capabilities and rehabilitation progress․ By identifying catastrophic thinking patterns, employers and healthcare providers can develop targeted interventions to enhance workplace accommodations, reduce absenteeism, and improve overall job performance․ This tool aids in creating personalized rehabilitation plans, fostering a smoother transition back to work and promoting long-term employee well-being effectively․
Role in Pain Management Programs
The PCS plays a crucial role in pain management by identifying catastrophic thinking patterns that hinder recovery․ It helps tailor interventions to address psychological barriers, enhancing the effectiveness of treatment plans․ By monitoring changes in catastrophizing scores, healthcare providers can assess progress and adjust therapies accordingly․ This tool is vital for improving emotional and functional outcomes, ensuring comprehensive care that addresses both physical and psychological aspects of pain․
The PCS is a valuable tool in pain assessment, offering insights into cognitive and emotional responses․ Future research should focus on refining the scale and exploring its applications in diverse pain management programs to enhance patient outcomes․
The Pain Catastrophizing Scale (PCS) is a widely used tool for evaluating negative cognitive and emotional responses to pain, such as rumination, magnification, and helplessness․ It provides a structured framework for understanding how individuals process pain, aiding clinicians in identifying maladaptive thought patterns․ The PCS is administered as a 13-item self-report questionnaire, with responses scored on a 5-point scale․ This assessment helps guide personalized treatment plans and monitor progress over time, making it invaluable in both clinical practice and research settings․
Future Research and Implications
Future research should explore the PCS’s application across diverse populations and settings, adapting it for cultural and demographic variability․ Integrating digital tools for real-time assessment could enhance its utility․ Investigating the PCS’s role in predicting long-term pain outcomes and its interaction with interventions like mindfulness or cognitive-behavioral therapies is crucial․ Expanding its use in non-clinical environments, such as workplace health programs, could broaden its impact․ These advancements will refine pain management strategies and improve patient care globally․
